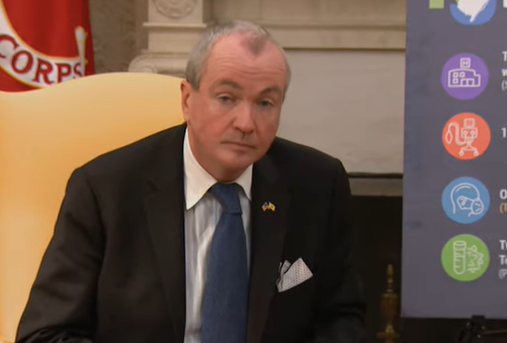
Governor Murphy Announces Departmental Actions to Increase Insurance Coverage to Cover Expanded Testing Access for COVID-19
Governor Murphy Announces Departmental Actions to Increase Insurance Coverage to Cover Expanded Testing Access for COVID-19
05/13/2020
“As we strengthen and expand New Jersey’s testing infrastructure,we must ensure that our residents are focused on their health and not on the cost of COVID-19 testing and related services,” said Governor Murphy. “These significant departmental actions are critical in improving affordability and alleviating costly financial burdens for New Jerseyans impacted by COVID-19.”
Departmental Actions
Department of Banking and Insurance
- Issued expanded guidance to carriers to ensure that policyholders are not charged out-of-pocket costs for testing, whether symptomatic or asymptomatic, regardless of where the test is administered.
- The guidance also requires that services provided to an individual during a visit that results in a test being ordered or administered, are also covered without any out-of-pocket costs to the policyholder.
Department of Health
- All federally qualified health centers (FQHCs) and acute care hospitals can submit the costs for COVID-19 diagnostic testing for individuals who have no other health care coverage to the Uncompensated Care Fund.
- Those costs will be reimbursed through the normal reimbursement procedures for the Uncompensated Care Fund. All health care facilities are encouraged to submit claims for testing uninsured individuals to the Health Resources and Services Administration COVID-19 Uninsured Program. The link to HRSA’s COVID-19 Claims Reimbursement Fund is: https://www.hrsa.gov/CovidUninsuredClaim
Department of Human Services
- NJ FamilyCare, including Medicaid, continues to cover testing without copayments or cost-sharing for beneficiaries, regardless of whether individuals are symptomatic.
Department of Treasury
- The State Health Benefits Program and School Employees’ Health Benefits Program are covering the cost of testing for symptomatic and asymptomatic beneficiaries. For Active and Early Retiree Populations that are serviced by Horizon and for the Retiree Population serviced by Aetna Medicare Advance (Part C), there will be no cost-share for member coverage of COVID-19 testing.
- For retirees covered through Medicare Advantage, their plans will cover the cost of COVID-19 testing with no cost-share for beneficiaries, regardless of whether individuals are symptomatic.
For more information on DOBI’s efforts, please click here.





